When people run into challenges navigating the health care system such as language barriers, help renewing their insurance or questions about their coverage, certified application counselors (CACs) are an invaluable resource. Recent federal changes to Medicaid and the Affordable Care Act (ACA) Marketplace will only create additional roadblocks to enrollment. These changes, including work reporting requirements, shortened enrollment periods and six-month redetermination requirements, are likely to further complicate the enrollment process and add more administrative barriers with narrowed time constraints, making the guidance of knowledgeable CACs not just helpful, but essential.
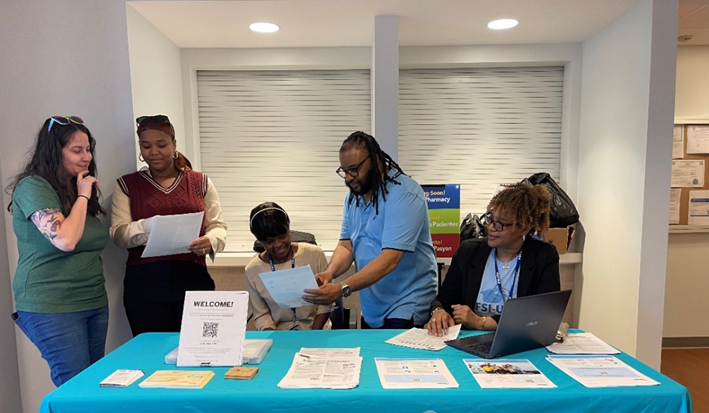
Since 2023, MassHealth and Health Care For All have been working in collaboration with 23 community-based organization (CBO) partners to train CACs to expand enrollment capacity in the 15 Massachusetts communities with the highest rates of MassHealth coverage. These CACs are embedded in their communities and proficient in multiple languages. As a result, they are able to bridge gaps in trust and accessibility. In recent months, the presence of immigration enforcement has led to fear and lower member turnout in the community, but the CBOs have continued to offer enrollment assistance and educate members about their coverage eligibility. A CAC from Brazilian Women’s Group recently reflected on their work, “Now more than ever, we are very important to [the Brazilian community]. With all the immigration issues, it helps for them to speak with someone in Portuguese and someone they can trust. It’s an honor to do this work.”
Recent changes surrounding Medicaid and Marketplace eligibility add an additional layer of confusion to an already uncertain time. Navigating changes like those in the federal budget reconciliation bill demands the kind of consistent guidance CACs provide. One of these new requirements is for Medicaid members to report 80 hours per month of paid employment, volunteer work or education. Commonly known as “work requirements,” this administrative hurdle will impede people from accessing coverage. According to recent data, an estimated 46% of MassHealth members would lose coverage despite 76% already working or meeting exemption criteria.
Additionally, annual redetermination cycles have been replaced in many states with six-month reviews leading to heightened churn. As a result, vulnerable individuals may lose coverage abruptly due to missed deadlines or documentation gaps.
It won’t only be Medicaid recipients who will experience significant changes, though. Community members who receive coverage through the ACA Marketplace will also face drastic alterations to their enrollment process. Enrollment periods for ACA Marketplace plans are being cut in half —from 90-day windows to as little as 44 days, beginning in 2026. Elimination of automatic re-enrollment will likely lead to confusion, missed deadlines and members falling off coverage. These policy shifts are poised to send ripples through health care nationwide, negatively impacting coverage rates. KFF estimates that policy changes to Marketplace eligibility and shortened enrollment windows could leave an additional 8.2 million people uninsured—with overall coverage losses possibly reaching 16 million when combined with Medicaid reductions.
As the American health care system reels from these announced federal enrollment changes, the role of CACs has become more essential than ever. Their presence ensures that our most vulnerable populations aren’t left behind, and HCFA is proud to support them as they continue this vital work. In an era where every missed deadline, lost subsidy or failed renewal can result in months without coverage, CACs aren’t just a convenience; they’re a lifeline.
Grace Jurkovich is a Policy Manager at Health Care For All.