June 27, 2022 – Ten years of legislative advocacy led by Health Care For All (HCFA) and our Oral Health Advocacy Taskforce (OHAT), resulted in the recent restoration of full Medicaid – known in Massachusetts as MassHealth – adult dental benefits. In January 2021, the MassHealth Dental Program started covering comprehensive dental care for all Medicaid patients, a big step towards increasing access to dental care. In addition to preventive care, exams, fillings, and extractions, MassHealth now includes root canals, crowns, periodontal services, and dentures.
However, many MassHealth patients continue to get care for non-traumatic dental conditions at the hospital emergency departments (EDs). Most of these ED visits are for problems that could have been treated at a dental clinic or even avoided with routine dental care.
Getting treatment for dental emergencies at an ED instead of a dental clinic is neither clinically effective nor cost-efficient. Most often, EDs do not have staff with dental training and are not equipped to provide comprehensive dental care. Most visits to the ED for dental conditions focus on pain management and do not resolve the problem, which will often return without treatment by a dentist. We also know that poor oral health is associated with life-threatening systemic diseases such as sepsis, diabetes, heart disease and lung disease, which further increases the health and cost burdens of untreated oral diseases. Moreover, the cost of an average visit at a dental office is between $90-$200, which is four to seven times less than that of an ED visit for a dental problem which ranges between $440-$1,500. Efforts to improve access to routine, preventive dental care may not only avoid future expensive ED visits but also improve people’s health and well-being.
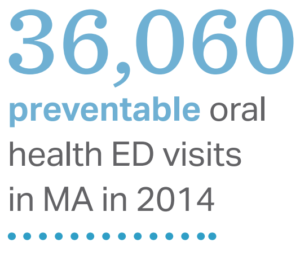
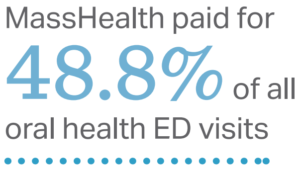
Despite the newly comprehensive MassHealth dental coverage, Medicaid patients in Massachusetts are visiting the ED for dental emergencies more frequently than the national average. Children covered by MassHealth visited the ED for oral health conditions close to 6 times more often than commercially insured patients, and that rate jumps to 7 times for non-elderly adults covered by MassHealth. Massachusetts Health Policy Commission (HPC) reported 36,060 ED visits for non-traumatic dental conditions in 2014, costing the health care system $14.8-$36 million.
MassHealth has an opportunity to help lessen this problem by investing in diverting dental patients from EDs to dental clinics. Two initiatives to tackle this problem are currently in their initial stages. First, OHAT is planning to conduct a campaign to raise awareness of the expansion of Medicaid adult dental benefits. The hope is that wider knowledge of the full range of covered dental services will encourage more patients to seek preventive and restorative care before dental emergencies arise. Second, MassHealth is aiming to start an ED referral program which will directly link patients who visit the ED for dental emergencies to dental clinics in their communities. Those dentists can then provide definitive treatment and help prevent further expensive ED visits. There has been no successful large scale implementation of similar programs in the U.S. so far. MassHealth’s ED referral program for dental conditions has great potential to prevent expensive and ineffective ED visits, improve health and well-being, and serve as an example for the rest of the country.
Ivy F. Lin is a dentist and 2022 MPH graduate of the Harvard T.H. Chan School of Public Health. As part of her MPH program, Dr. Lin completed a practicum project with MassHealth and HCFA.
**To learn more about our oral health coalition (OHAT), please email HCFA’s Oral Health Director, Dr. Samantha Jordan, at samjordan@hcfama.org.
**If you are interested in joining our OHAT campaign to raise awareness of the expansion of Medicaid adult dental benefits: please share your interest here.

